Has walking, standing, sitting, or climbing stairs been leaving you with stiffness or discomfort around your hips or lower back? If so, you are not alone. Hip pain is a common complaint, and its source is not always as straightforward as it may seem.
At a recent OrthoUnited community discussion, Dr. Dean Marshall, DO, walked attendees through how physicians evaluate hip pain and why accurately identifying the source of symptoms is essential for effective treatment. Understanding where pain originates allows providers to tailor care appropriately and avoid unnecessary or ineffective interventions.
Below is an overview of how hip pain is evaluated, based on Dr. Marshall’s clinical approach and discussion.
The Possible Sources of Hip Pain: Likely Culprits
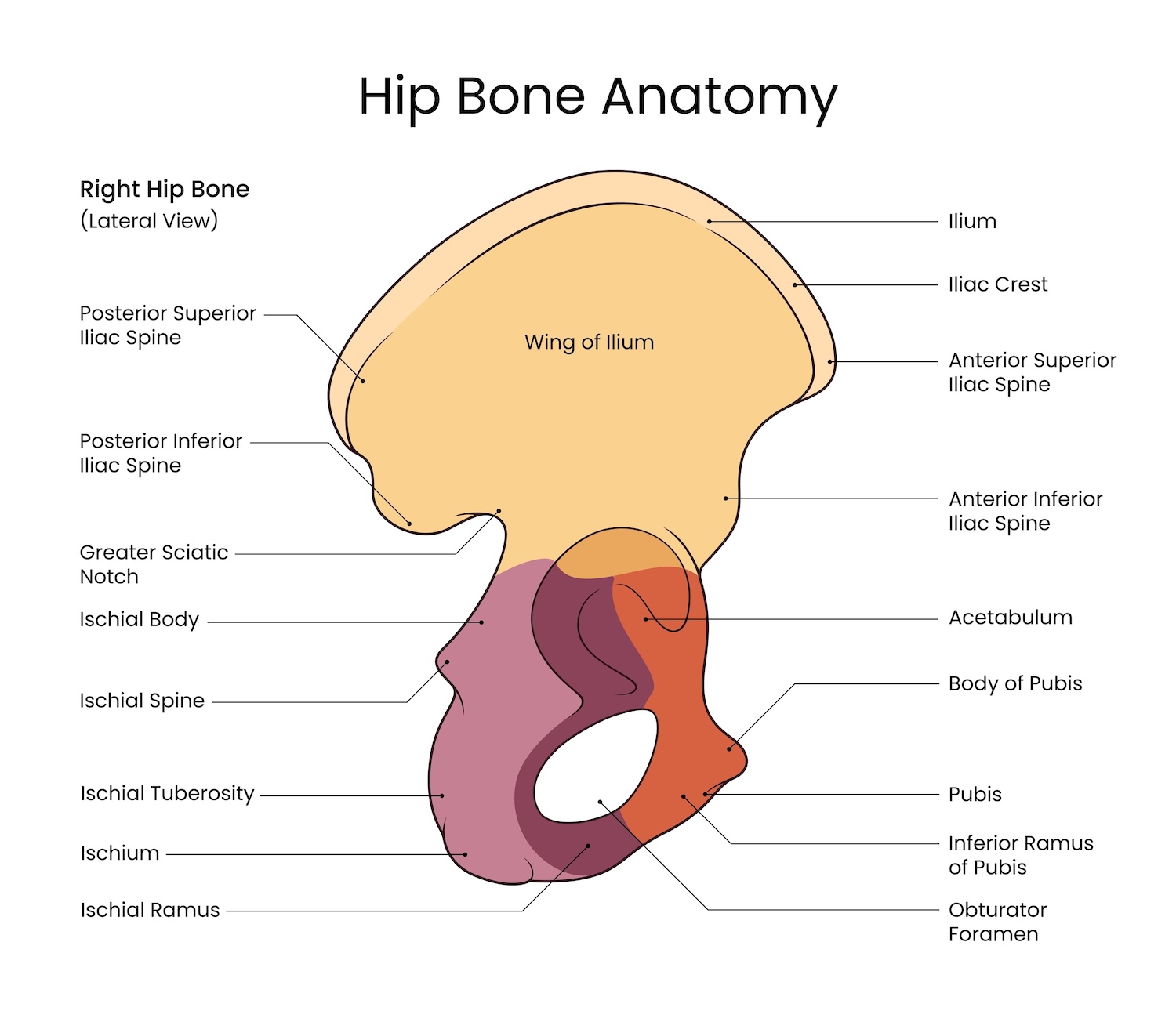
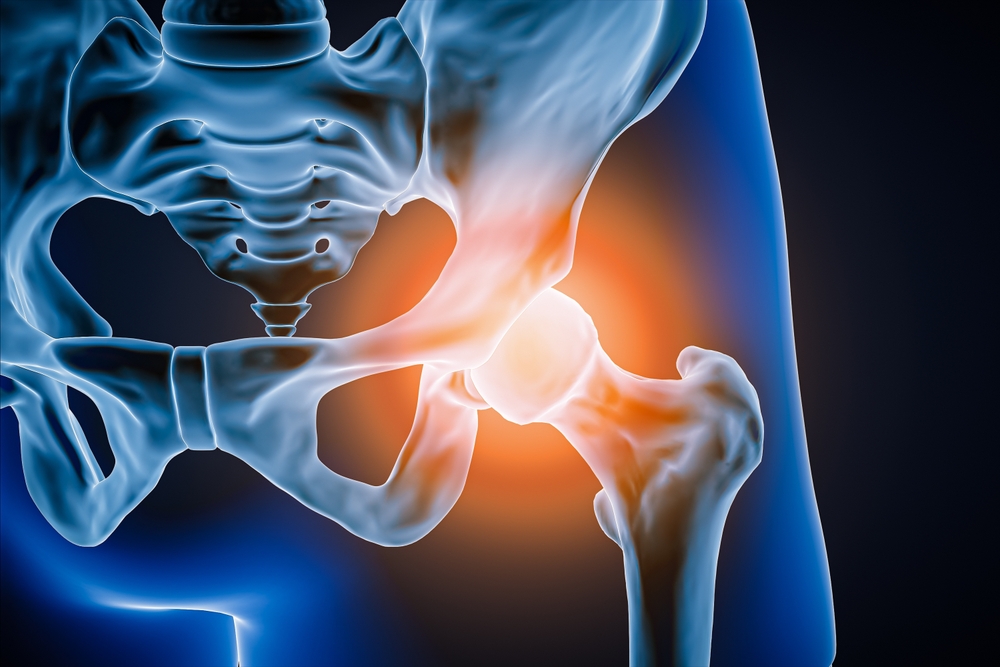
The hip region is a complex area made up of bones, cartilage, muscles, tendons, ligaments, and nearby nerves. Pain can arise from structures within the hip joint itself, from tissues surrounding the joint, or from areas outside the hip that refer pain to this region.
Intra-Articular Sources
Intra-articular conditions involve structures inside the hip joint, including:
- The labrum, a ring of cartilage that helps stabilize the hip socket
- Articular cartilage lining the joint surfaces
- Bony abnormalities such as femoroacetabular impingement (FAI)
- Degenerative changes from early to advanced osteoarthritis
Pain from intra-articular sources is often felt deep in the groin or the front of the hip. Patients may describe aching, catching, or clicking sensations. Symptoms frequently worsen with hip flexion, twisting movements, prolonged sitting, or athletic activities that require pivoting.
Extra-Articular Sources
Extra-articular conditions originate in the soft tissues surrounding the hip joint. Common examples include:
- Gluteal tendinopathy, involving the tendons of the gluteus medius and minimus muscles
- Trochanteric bursitis
- Iliotibial band irritation
Pain from these conditions is typically located along the outer hip or lateral thigh. It may worsen when lying on the affected side, climbing stairs, walking long distances, or standing on one leg. Dr. Marshall emphasized that what was once broadly labeled as “trochanteric bursitis” is now more often understood to be tendon-related rather than isolated bursal inflammation.
Referred Sources
Not all hip pain originates in the hip. Referred pain may come from:
- The lumbar spine
- Nerve root irritation
- The sacroiliac (SI) joint
- Occasionally, abdominal or pelvic structures
These sources can mimic hip pathology. Symptoms may include buttock pain, pain radiating down the thigh or leg, or associated numbness and tingling. Recognizing referred pain patterns helps prevent misdiagnosis and ensures the correct area is treated.
How Pain Location Guides Evaluation
The location of pain offers valuable clues. Groin pain often points to intra-articular joint problems. Lateral hip pain commonly suggests gluteal tendon pathology or related soft tissue irritation. Pain in the buttocks or pain that travels down the leg raises concern for spine or SI joint involvement.
While these patterns are helpful, Dr. Marshall noted that many patients have overlapping features. A thorough evaluation is needed to determine the primary driver of symptoms.
What Doctors Ask During an Evaluation
A detailed medical history is a critical first step. Physicians typically ask:
- When the pain began, and whether it started suddenly or gradually
- Which activities or positions worsen or relieve symptoms
- Whether there are mechanical symptoms such as popping, clicking, or locking
- If pain disrupts sleep, particularly when lying on one side
- Whether there is radiation into the leg, numbness, or tingling
- If there is a history of back pain, sciatica, or spinal conditions
These questions help narrow the list of possible causes before the physical exam begins.
What Doctors Look for During a Physical Exam
The physical exam is designed to reproduce symptoms and assess how different structures respond to movement and stress.
Intra-Articular Hip Evaluation
Physicians assess range of motion, paying close attention to pain with hip flexion and internal rotation. Provocative tests such as FADIR and FABER can help identify impingement, labral pathology, or joint irritation. Pain reproduced with passive motion or axial loading also suggests intra-articular involvement.
Gluteal Tendinopathy Evaluation
For suspected gluteal tendon pathology, clinicians palpate the greater trochanter to check for localized tenderness at the tendon insertion. Functional tests, such as a single-leg stance or Trendelenburg test, may reveal pain, weakness, or reduced endurance of the hip stabilizing muscles. Resisted hip abduction or external rotation often reproduces symptoms.
Hamstring Tendinopathy Evaluation
Hamstring-related pain is typically located near the gluteal fold. Symptoms may worsen with hip flexion combined with knee extension, and tenderness is often present at the proximal hamstring origin.
Lumbar Spine and SI Joint Evaluation
When spine or SI joint involvement is suspected, doctors may perform straight-leg raise testing, neurologic exams assessing strength, reflexes, and sensation, and SI joint stress maneuvers such as compression, distraction, or thigh thrust tests.
Diagnostic Tools Used To Confirm the Source
Imaging and targeted interventions help confirm clinical findings.
- X-rays evaluate joint space narrowing, arthritis, and bony morphology, and are essential when considering hip replacement.
- MRI provides detailed views of soft tissues, allowing visualization of labral tears, cartilage damage, tendon degeneration, or inflammation.
- Image-guided injections can be both diagnostic and therapeutic. Temporary pain relief following an injection helps confirm the structure responsible for symptoms.
Treatment Options: Nonoperative to Operative
Most patients improve with conservative care. Common nonoperative treatments include:
- Activity modification and rest
- Physical therapy focused on movement control and strength
- Anti-inflammatory medications
- Progressive loading programs, including isometric and eccentric exercises
In some cases, injections, platelet-rich plasma (PRP), or other biologic treatments may be considered, particularly when inflammation contributes to pain. Dr. Marshall noted that these options may reduce symptoms but are not a cure for structural problems.
When symptoms persist despite appropriate nonoperative care, surgical treatment may be discussed. Options depend on the underlying diagnosis and severity of the disease.
Surgical Options
- Hip arthroscopy may address labral tears or bony impingement
- Gluteal tendon debridement or repair may be considered for refractory gluteal tendinopathy
- Total hip replacement is reserved for advanced arthritis or irreparable joint damage
Surgery is typically considered only after conservative measures have failed and imaging findings correlate with symptoms.
Ready to Take the Next Step?
If you are living with hip pain, you do not have to manage it alone. OrthoUnited’s hip specialists offer comprehensive evaluation and personalized treatment plans designed to identify the true source of your pain and help you move more comfortably.
Give us a call or schedule an appointment online to start your journey toward recovery.
Learn More Through OrthoUnited Community Events
OrthoUnited’s free, community discussions give patients the opportunity to learn directly from physicians and better understand how orthopaedic conditions are evaluated and treated. These educational events provide a supportive environment to ask orthopaedic specialists questions and gain clarity about musculoskeletal health.
If you are interested in learning more about hip pain or other orthopaedic topics, we invite you to attend a future community discussion. This series is offered as a free educational resource to support the health and well-being of Northeast Ohio.